POTS covers quite a broad array of symptoms. What is prominent for one person, may not be such an issue for another. Treatment options are also extensive. There is no cure for POTS, and what works well for one patient, may actually make another worse. Subsequently, experiences of dealing with POTS can be varied, so what I may write might not be suitable or relevant for you.
As the name suggests, Postural Orthostatic Tachycardia Syndrome revolves around an issue with an abnormally increased heart rate when changing position, typically from supine to upright.
When all humans stand, gravity causes a shift in blood from the head to the lower parts of the body. In a healthy person, the heart rate increases slightly, the heart pumps stronger, and the vessels in the lower part of the body constrict, all ensuring the blood is pushed back up to maintain a healthy blood flow in all parts of the body. This all occurs in about 2 heart beats.
 In someone with POTS, the heart rate increase does not result in improved blood flow, the vessels often do not contract efficiently, the blood pressure may drop drastically, and the heart rate continues to increase. There is then a decrease in cerebral blood flow, resulting in light headedness or fainting. The high heart rate is considered to be a sign of POTS when it is increased by more than 30 beats per minute upon standing, or to a heart rate greater than 120 beats per minute within 10 minutes of standing still.
In someone with POTS, the heart rate increase does not result in improved blood flow, the vessels often do not contract efficiently, the blood pressure may drop drastically, and the heart rate continues to increase. There is then a decrease in cerebral blood flow, resulting in light headedness or fainting. The high heart rate is considered to be a sign of POTS when it is increased by more than 30 beats per minute upon standing, or to a heart rate greater than 120 beats per minute within 10 minutes of standing still. Although POTS is an issue which results in a heart rate and blood pressure issue, it is not actually a problem with the heart. The problem is with the autonomic system, which is the body's involuntary nervous system that controls the actions that we do not need to think about, such as sweating, breathing and heart rate.
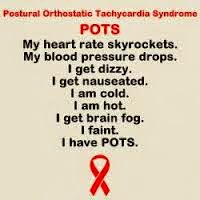
As well as pre syncope, fainting, a racing heart and palpitations, POTS can cause many other symptoms. These can include nausea, unrelenting fatigue, exercise intolerance, post exertion malaise, headaches, migraines, shaking, sweating, weakness, discolouration of limbs from blood pooling, anxiety, chest pains, visual disturbances, poor sleep, shoulder and neck pain, abdominal discomfort and digestion issues, temperature control disturbances, and brain fog (poor concentration and memory). These symptoms, although worse when moving into an upright position, are often present constantly.
Usually the cause of POTS in an individual can not be identified or treated. It can be something transient like a virus, trauma or pregnancy. For some people, the cause could be another condition, like joint hypermobility syndrome (Ehlers-Danlos) or autoimmune diseases, so concentrating on these issues may see an improvement in the POTS symptoms. Other causes may included spinal stenosis and deconditioning.
As there is no cure for POTS, treatment is a matter of dealing with each symptom. Generally, the first changes to be made concentrate on lifestyle. Ideas such as the following can be helpful:
- Dehydration reduces the blood volume in the body, so it is very important that people with POTS maintain good hydration, and increase salt intake (generally 2-4 grams per day - do so only under doctor's supervision though).
- Heat and alcohol cause dilation in blood vessels so avoiding these where possible can help. Use personal cooling devices, or fans and air conditioning where possible.
- Eating large, heavy meals diverts blood away from the brain to concentrate in the gut, so eat small, frequent meals instead. Looking at certain foods which may be triggers for some people is also worth investigating with a nutritionist.
- Compression stockings can help the blood flow in the legs, as can strong calf muscles and general fitness. Exercise is very difficult for people with POTS, and trying to find something that suits each individual is a matter of trial and error. Swimming can be good, as can seated exercise, like a recumbent bike or rowing machine, or gentle stretching or yoga.
- Elevating the whole bed so that the head end is 4-12 inches higher than the feet is useful for some patients with low blood pressure or volume.
- Standing and sitting for long periods causes symptoms for most POTS patients, so avoid these situations. Lying down and elevating legs can avoid light headedness or fainting. If unable to do this, try crossing the legs and squeezing the thighs together and clenching the buttocks and fists, or other counter manoeuvres which help to decrease the amount of blood pooling in the legs. Changing positions slowly, i.e. from lying/sitting to standing, will help the body adjust too.
- People with POTS often require more rest and sleep than normal.
- Identifying triggers by using heart rate monitors/watches can be useful.
- Most people with POTS describe symptoms to be worse in the morning, so planning activities in the afternoon or evening can be helpful.
- Showering can be problematic due to the heat, prolonged standing, and general exertion. Sitting can improve this, as can using cooler water. Running cold water on the legs before leaving the shower can constrict the blood vessels to help with blood flow.
I was diagnosed a year ago, but have had symptoms since I was quite young. I have tried so many of the above treatment options, and am yet to see enough improvement to return to a normal quality of life. For me, fatigue, poor exercise tolerance, post exertion malaise, and light headedness (including pre syncope, dizziness and visual disturbances) are my most debilitating symptoms. These mean that I can not work or drive, or live independently. I also often have brain fog, nausea, headaches, pain, my sleep routine is poor, and I have digestion issues. I do get all the other symptoms on the list too, to varying degrees and frequency (including altered temperature control, however this one usually effects people around me more than me, because when they are near me, they either complain about how freezing cold or how boiling hot I am to touch, and I am quite oblivious to it!!).
2014 was filled with medication trials. Most made me feel really bad, and one has made a slight difference. I have a new list of medication options to start soon, so unfortunately it looks like another year ahead filled with medication trials. Hopefully, more successful than last year's! If I can find medications which enable me to be well enough to do some exercise, I can work to become stronger and fitter, which is also important in improving my situation. Then I can work towards being more independent. It is a very slow and excruciating process, but hopefully worth it in the end.
 Having POTS is definitely no walk in the park. For some people it can be mild, for others, like myself, it stops them from being active and independent, and others are restricted to a wheelchair. It is quite a rollercoaster, as some days you can feel slightly better and become hopeful for improvement, only to plummet down into feeling bad. It is also frustrating, disheartening and lonely, because you often can not do what you want, when you want. People around you often do not understand your situation, as you "look normal," and for the most part, you try your best to not let on how you are feeling. Many opportunities are missed, and you can end up feeling like life is passing you by.
Having POTS is definitely no walk in the park. For some people it can be mild, for others, like myself, it stops them from being active and independent, and others are restricted to a wheelchair. It is quite a rollercoaster, as some days you can feel slightly better and become hopeful for improvement, only to plummet down into feeling bad. It is also frustrating, disheartening and lonely, because you often can not do what you want, when you want. People around you often do not understand your situation, as you "look normal," and for the most part, you try your best to not let on how you are feeling. Many opportunities are missed, and you can end up feeling like life is passing you by. However, as with most negative situations, there is a lot to learn and strength to be gained from it. My life has changed drastically because of POTS, but I am hopeful that I will gain control of it at some point. I also have new paths to venture down in life that I would not have looked at had this not happened to me. As disappointing and frustrating as it is, I have to look at it that these new options are the positives from a bad situation.
There are many good articles out there that discuss POTS. I particularly think these two explain it well, and the options available:
http://circ.ahajournals.org/content/117/21/2814.full


Such a comprehensive and important explanation of your condition Gem. This must give comfort to those people out there who have been diagnosed and their loved ones who may have been suffering from a lack of knowledge &, therefore, empathy.
ReplyDeleteI take my hat off to you.
Thank you for your ongoing support Dean. I really do hope that this explanation may help someone. It also gives me comfort that fellow nurses are reading this and learning a little more about a condition we often do not hear much about. This gives me hope that more patients will gain the support and care they deserve.
Delete